Digital pathology and AI: your guide to basics and beyond
This is your guide to digital pathology and artificial intelligence. Learn everything essential, from benefits and challenges to current trends and solutions.
This is your guide to digital pathology and artificial intelligence. Learn everything essential, from benefits and challenges to current trends and solutions.
Digital pathology is the process of digitizing pathology slides for analysis. The glass slides containing tissue sections are scanned with high-resolution scanners to create digital images of the tissue. These images can be viewed, analyzed, and shared electronically using specialized software. Digital pathology offers several advantages over traditional microscopy, including the ability to easily store, retrieve, and share images and the potential for automated image analysis and quantification.
In 2018, there were an estimated 18.1 million new cancer cases worldwide. WHO predicts that global cancer cases per year will have increased to 29.4 million by 2040, with the most significant increases in low and middle-income countries.1
The shortage of pathologists has been detected in certain areas of the medical industry. This, combined with growth in the number of samples, could lead to pathologists being overworked. The need for pathologists, especially those with AI and digital pathology skills, will continue to increase.2, 3, 4
Expansion in digital pathology is widespread as the adoption of microscope scanners to convert samples into digital images is increasing. This makes it possible for laboratories to adopt AI to improve the efficiency and reliability of workflows. The use of AI in pathology is expected to dominate the field in the upcoming years.5 The global AI in pathology market is predicted to have an average annual growth rate (CAGR) of 15.6% between 2023 and 2028.6
Understanding how an AI model works is essential for ensuring its safety and effectiveness. Pathologists are always in control, and when making the final decision, they must trust the AI's recommendations and understand potential limitations.7 The concept of transparent AI can be broken down into explainability (understanding how the AI arrived at a specific output), data clarity (knowing what data was used for training and what data is currently being used to make decisions), and open communication (companies being open about the AI's capabilities, limitations, and potential impact).
The Royal College of Pathologists8 lists four aspects impacted by digital pathology:
Read more benefits from this blog: The benefits of digital pathology
.png?width=395&height=255&name=Malm%C3%B6%20at%20Region%20Sk%C3%A5ne%20pathology%20lab%2c%20Sweden%20(1).png)
Several studies have estimated cost savings of more than $250,000 per institution per year as a result of implementing digital pathology.9 However, getting started requires a substantial investment that can be a barrier for organizations with limited budgets or inadequate IT support. Healthcare providers in developing countries are especially struggling with financial constraints that prevent them from adopting digital pathology.6 Regional and national funding programs and initiatives have been supporting the investments in many regions. One example is the UK, where the National Health Service (NHS) has received much financial support from the government.10-11
The evolving landscape of data security regulations and guidelines from regulatory bodies requires constant vigilance from digital pathology vendors. Adapting to new requirements and ensuring ongoing compliance can demand significant resources and expertise.
Clear quality control measures are essential to ensure the reliability and accuracy of results when using AI in digital pathology. Significant drift in the protocols, procedures, and data sets is likely to affect the performance of an AI model, which may require additional training to compensate for these changes.
Adopting new practices necessitates a change in mindset. Implementing digital pathology may require significant changes to laboratory workflows and, thus, pathologists' daily routines. The importance of adequate training and available support cannot be overstated during and after implementation.
Integrating digital pathology systems into existing laboratory infrastructure can be complex. Choosing a partner who understands the importance of integrations and has executed successful implementation projects is vital. At Aiforia, a specialized integration team ensures that the Aiforia® Platform is seamlessly integrated into existing digital pathology systems (LIS, LIMS, PACS, IMS, scanners) to enable automated and optimal workflows.
Skåne, a southern county of Sweden, completed one of the world's largest adoptions of digital pathology in 2019-2020. Four labs, 14 scanners, and an estimated 890,746 slides were used and scanned from May 2019 to July 2020.
“We initially had to update all the technical infrastructure, like graphics cards, monitors, everything. At some labs, we even had to update their wireless networks”, Kevin Sandeman, Department Manager at Region Skåne’s pathology lab in Malmö, Sweden, comments. He was at the helm of this feat, pushing forward the digitization of these pathology labs.
If your organization is considering starting a digitalization process, Dr. Sandeman advises to “involve the pathologists early on in the development of the applications and the flow so they have the possibility to influence the process from the beginning.”
Read the full story here: Case Skåne: one of the world’s largest digital transformations in pathology
Azienda Zero, the broadest public healthcare provider in Veneto’s North Italian region, aims to create a safe, standardized process to improve patients’ clinical care with their ongoing digitalization project.
These eight components are covered in the digital pathology transformation project in Veneto:
Read the full story here: Digital pathology deployment in Veneto: 8 steps to success
Digital pathology has paved the way for artificial intelligence to further advance sample image analysis and optimize the efficiency of diagnostic workflows. Deep learning, a subset of machine learning that falls under the AI category, is setting new records and high standards in fields such as image recognition.
Some of the most significant benefits of deep learning AI in pathology are:
Increased accuracy and time-savings
Increased efficiency in diagnostic laboratory workflows and research and discovery
Increased consistency and reliability
Increased possibilities to build prognostic and predictive tools to suggest treatment paths for patients
Improved research methods to make novel findings to understand disease mechanisms better
“There is potential for AI to support the diagnostic process in pathology, particularly image analysis in histopathology, where it can detect disease, grade its severity, and possibly predict treatment response.” – The Royal College of Pathologists
Learn more about how deep learning is transforming digital pathology >


The digitalization project starts with microscope scanners, as the central step in digital pathology is getting the samples into a digital format for further analysis. During scanning, the CCD camera takes single pictures of small tissue areas that subsequently undergo complex postprocessing steps to produce the complete whole slide image (WSI). Good-quality images are crucial for analysis in the later stages of the workflow.

An image management system (IMS) is used for storing, organizing, and viewing digital sample slides. It must be able to handle large file sizes, support various image formats, and integrate with other lab systems.
Scanning and digitizing the microscope slides generates vast amounts of data, which would be impossible to handle without modern information technology. Thus, secure and scalable image management and storage play essential roles in digital pathology workflow.
Example: A medium-sized diagnostic pathology lab with 7000 biopsy cases, with an average of 4 slides per case, produces 28,000 sections per year and thus requires at least 11 TB storage space per year (average file size = 400 MB) if all slides are scanned only at 200x magnification. In comparison, the same storage space would be needed for 1833 full HD movies (6 GB each).

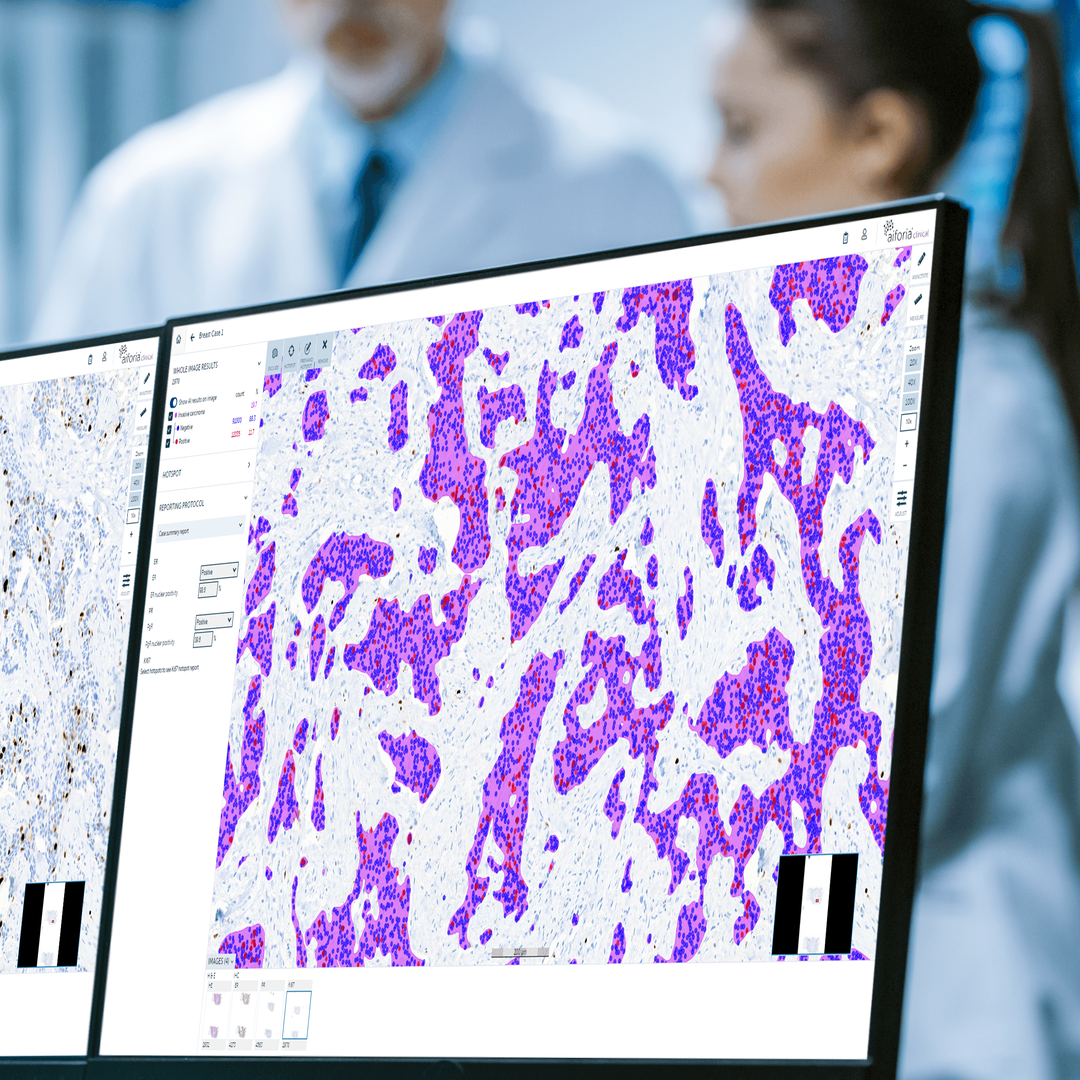
These systems display digital slides with sufficient detail for accurate diagnosis. Different AI models are leveraged to analyze the sample slides, assisting pathologists in tasks such as cell counting, tumor measurements, tumor grading, and biomarker detection and quantification.
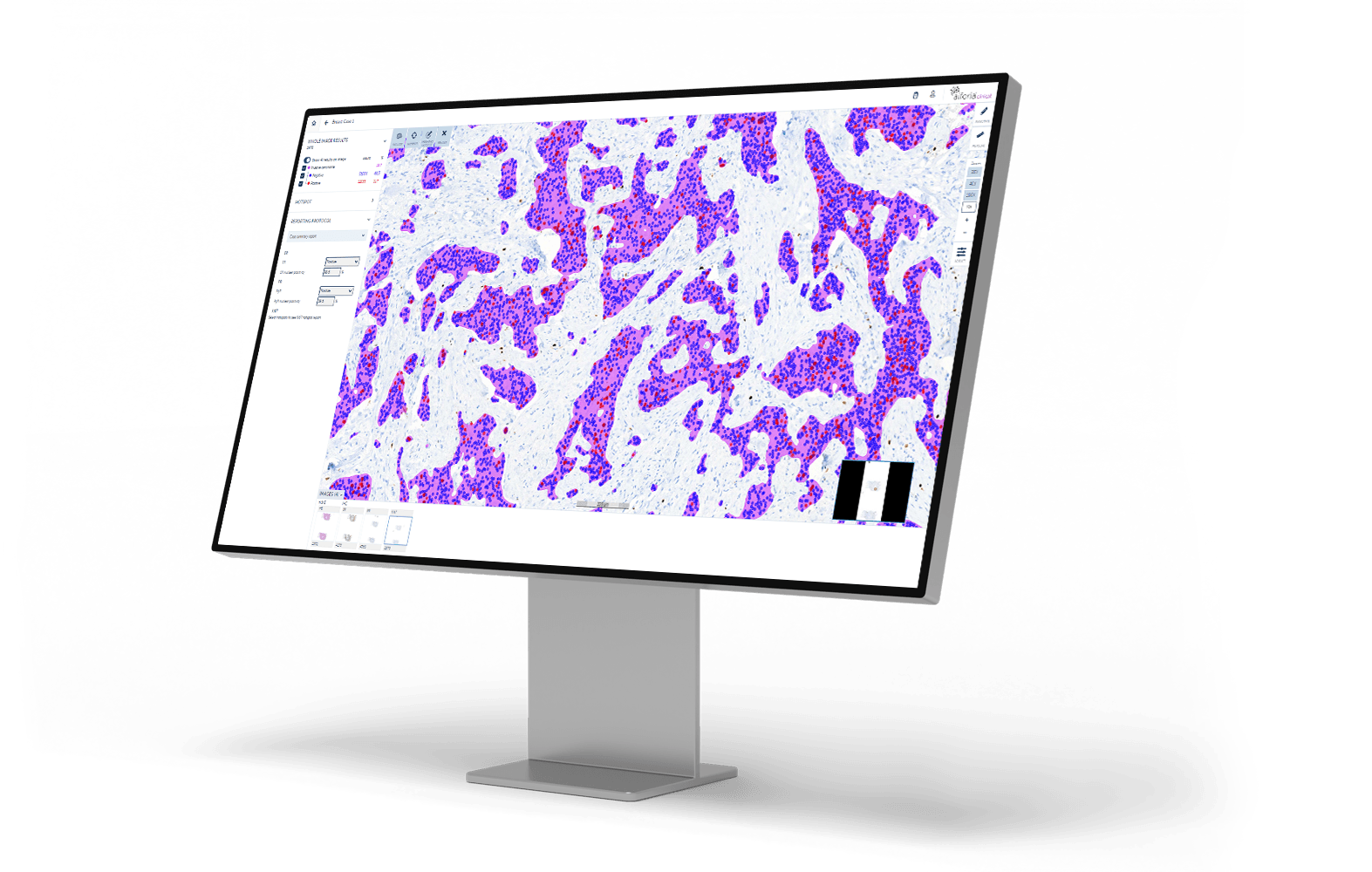
The importance of an AI-driven, interactive user interface cannot be stressed enough in this context. Aiforia’s AI models serve as first-read support while the expert verifies the results. We offer our customers fully quantifiable data and results that can easily be adjusted in an interactive user interface, which helps the pathologist to review areas of interest and complete the case review rapidly.
Explore Aiforia's solutions for a multitude of industries and use cases:

The digitalization project starts with microscope scanners, as the central step in digital pathology is getting the samples into a digital format for further analysis. During scanning, the CCD camera takes single pictures of small tissue areas that subsequently undergo complex postprocessing steps to produce the complete whole slide image (WSI). Good-quality images are crucial for analysis in the later stages of the workflow.

An image management system (IMS) is used for storing, organizing, and viewing digital sample slides. It must be able to handle large file sizes, support various image formats, and integrate with other lab systems.
Scanning and digitizing the microscope slides generates vast amounts of data, which would be impossible to handle without modern information technology. Thus, secure and scalable image management and storage play essential roles in digital pathology workflow.
Example: A medium-sized diagnostic pathology lab with 7000 biopsy cases, with an average of 4 slides per case, produces 28,000 sections per year and thus requires at least 11 TB storage space per year (average file size = 400 MB) if all slides are scanned only at 200x magnification. In comparison, the same storage space would be needed for 1833 full HD movies (6 GB each).

These systems display digital slides with sufficient detail for accurate diagnosis. Different AI models are leveraged to analyze the sample slides, assisting pathologists in tasks such as cell counting, tumor measurements, tumor grading, and biomarker detection and quantification.
The importance of an AI-driven, interactive user interface cannot be stressed enough in this context. Aiforia’s AI models serve as first-read support while the expert verifies the results. We offer our customers fully quantifiable data and results that can easily be adjusted in an interactive user interface, which helps the pathologist to review areas of interest and complete the case review rapidly.
Explore Aiforia's solutions for a multitude of industries and use cases:
World Health Organization. (2020). WHO report on cancer: setting priorities, investing wisely and providing care for all. https://www.quotidianosanita.it/allegati/allegato4849716.pdf
Bychkov, A. & Fukuoka, J. (2020, March). Evaluation of the global supply of pathologists. United States & Canadian Academy of Pathology 111th Annual Meeting. http://dx.doi.org/10.1038/s41379-022-01050-6
The Royal College of Pathologists. (2024). The pathology workforce. https://www.rcpath.org/discover-pathology/public-affairs/the-pathology-workforce.html
Prajapati, P. R. et al. (2023). Pathologists Shortage in United States of America (USA) - How Academic Centers and Private Laboratories Can Play an Effective Role in Recruiting Qualified Future Pathology Residents from Pool of United States (US) and International Medical Graduates (IMGs). American Journal of Clinical Pathology 160(1), 65-66. https://doi.org/10.1093/ajcp/aqad150.146
Emad, A. R. et al. (2021). Current and future applications of artificial intelligence in pathology: a clinical perspective. Journal of Clinical Pathology 74(7), 409-414. https://doi.org/10.1136/jclinpath-2020-206908
MarketsandMarkets Research Private Ltd. (2023, July). AI in pathology market size, share & trends by component (software, scanners), neural network (CNN, GAN; RNN), application (drug discovery, diagnosis, prognosis, workflow, education), end use (pharma, biotech, hospital labs, research), & region - global forecast to 2028. https://www.marketsandmarkets.com/Market-Reports/ai-in-pathology-market-86647266.html
Jackson, B. R. et al. (2021). The Ethics of Artificial Intelligence in Pathology and Laboratory Medicine: Principles and Practice. Academic Pathology 8. https://doi.org/10.1177/2374289521990784
The Royal College of Pathologists. (2024, October 11). Digital pathology. https://www.rcpath.org/profession/digital-pathology.html
Patel, A. et al. (2021). Contemporary Whole Slide Imaging Devices and Their Applications within the Modern Pathology Department: A Selected Hardware Review. Journal of Pathology Informatics 12(1), 50. https://doi.org/10.4103/jpi.jpi_66_21
Evenstad, L. (2024, January 4). Government to push NHS roll-out of digital pathology. ComputerWeekly.com. https://www.computerweekly.com/news/366565535/Government-to-push-NHS-roll-out-of-digital-pathology
Department of Health and Social Care. (2020, August 29). Funding boost for artificial intelligence in NHS to speed up diagnosis of deadly diseases. Gov.uk. https://www.gov.uk/government/news/funding-boost-for-artificial-intelligence-in-nhs-to-speed-up-diagnosis-of-deadly-diseases